More Information
LASER is an acronym for: Light Amplification by the Stimulated Emission of Radiation
Broadly speaking, a laser is light energy that is reflected through a gain medium then multiplied between two mirrors in an optical cavity and the released emitting a coherent and monochromatic light either pulsed or continous, which depending on the wavelength and power, can perform a specific task
The wavelength can be better understood if we think of the colors of the rainbow or light spectrum: the gain medium or filter that the light goes through determine the wavelength.
The secret of using light energy for pain relief and acceleration in healing is the deep penetrating capability of laser light: if you can not hit the tissue you can not effect the tissue
The term laser conjures up in most people's minds a star wars type of weapon vaporizing anything in its path! Such lasers do, of course, exist that are capable of producing that effect. Yet, lasers have been in used in various fields of medicine since the early 1960's with great success. Lasers of this variety have proved to be invaluable in these fields as well: (1) Gynecology for treating cancer of the cervix, where accuracy and instant effective treatment is vital and (2) ophthalmology, dermatology, gastro-enterology, and otolaryngology.
Traditional Laser therapy is a safe, effective, noninvasive way to treat musculoskeletal injuries. It has been proven and approved by the United States FDA since 2003.
Traditional Laser therapy has successfully helped thousands of people with many debilitating conditions. It has been and continues to be used in hospitals and clinics in many countries. The technology is relatively new to the USA and most doctors do not know very much about the lasers available, the correct outputs, and wavelengths. Additionally, like computer technology, laser technology has made some quantum leaps in the past few years.
Therapy Lasers traditionally were using extremely low powers and short wavelengths which have caused penetration and efficacy issues for deep seated pathologies. New equipment and new protocols have lead to great success with many conditions thought to be untreatable or to painful for conservative treatments.
Additionally, laser therapy can be used when other modalities are contraindicated such as with pacemakers and over metallic implants. Laser therapy can be used to give immediate relief of painful conditions and accelerate healing.
The main problem with traditional laser therapy is tissues cannot be affected unless they can be reached by the laser. While there are thousands of studies to prove lasers can heal, the greatest scientific challenge of laser therapy is how to deliver the energy to the deep tissues without over heating the superficial tissues.
AHL has found the answer, thanks in part to partnership with Lucio Zagato at ASA in Italy and due to the patented protocols developed by Dr Bradley Frederick, Director of Dr. Leroy Perry’s International Sportscience Institute.
AHL has taken the world’s most powerful and safest laser delivery system, combined it with non- surgical cooling and active release technology to create the world’s most effective laser therapy system.
Whereas traditional laser therapy may take 20-30 visits and still be ineffective on deep tissue pathologies, AHL high intensity laser therapy( HILT) with AHL protocols is the only high powered laser that not only delivers immediate 20-30 percent pain relief, it can also be used for the deepest pathologies.
Because of the depth of penetration, quantity and quality of the AHL laser systems, not only is healing accelerated, the number of treatments required is decreased.
Included in AHL protocols are scientific pain and pressure measurements to insure recovery is on track. We can tell exactly when a professional athlete is ready to return to sports.
Furthermore, AHL’s patented High powered laser delivery system is the only high intensity laser that can be used on acute pathologies. With the ability to photocoagulate, it stops the swelling that leads to prolonged healing.
Each treatment is less than 15 minutes, is totally painless and continues to accelerate healing for up to 24 hours.
Lasers emitting blue/green visible light are used in ophthalmology and dermatology, where the beam is absorbed by the red pigmentation in the blood.
Low power red visible light would however commonly be used in dermatology for top surface skin repair such as burns, where the depth of penetration of the beam is minimal.
Lasers used in physiotherapy can also be low powered and most operate in the near infrared part of the light spectrum, producing invisible light waves.
This is the optimal wavelength for use in physiotherapy as the physiotherapist can achieve very good penetration which is vital in treating a variety of soft tissue problems.
In general the higher the wavelength, the deeper the penetration.
- Studied in Europe for past 25-30 years and in the USA the past 15-20 years
- 1960's:
- Term 'laser therapy' coined when it was noticed that irradiation with a laser light lead to enhanced wound healing
- Theodore Maiman brought first ruby laser into medicine
- Endre Mester (Hungary), grandfather of Photobiomodulation (laser therapy), reported on wound healing through laser therapy
- February 2002: the MicroLight 830 (ML830) received FDA approval for Carpal Tunnel Syndrome Treatment
- 2005: the world’s longest wavelength, deepest penetrating high powered laser received FDA approval
- 2008:
- AHL was founded by Dr. Bradley Frederick, who began designing patented protocols for the treatment of deep pathologies like osteoarthritis and acute sport injuries, and began training doctors and physiotherapists on these new techniques and the proper use of high powered lasers
- AHL started training doctors and physiotherapists on these new techniques and the proper use of high powered lasers.
The term laser therapy was coined in the early 1960’s when it was noticed that irradiation with a laser light lead to enhanced wound healing.
It was Theodore Maiman in the early 1960’s who brought the first ruby laser into medicine.
Laser therapy would begin a few years later when a Hungarian physician named Endre Mester, while using an under powered laser to kill cancer cells in rats, observed an increase in wound healing. He is now considered the grandfather of Photobiomodulation also known as laser therapy.
Early research was focused on very low powered lasers (power outputs less than 500 milliwatts). In fact most of the original therapeutic lasers used powers less than 30 milliwatts. Again, the problem with these lasers is that they worked well for superficial healing; however, if one is to affect the cells, the laser light energy must come into contact with the cells.
Thus given the depth of penetration problem, the effectiveness of these first generation lasers was amazing. To date there have been more than 2,500 studies that have proven the efficacy of laser therapy. Over 200 of these studies were double blind control studies, yet acceptance in the USA is still limited. At AHL, we believe this is due in part to the fact that most lasers on the market have too little power to penetrate deep into human tissue. One only needs to look at the research to see that most laser studies have been done in vitro, meaning they did not have to penetrate the dermis, fascia, or muscle tissues.
Presently, hundreds of lasers are on the market. However, like all technology, therapeutic lasers have become more and more sophisticated and powerful. At AHL, we have moved far beyond the first generation lower level lasers to higher wavelength and higher powered lasers.
At AHL, we began with the only FDA approved laser. However, after hundreds of cases we noticed it was more effective on superficial injuries. In an effort to deliver more energy we stared using multiple lasers at one time. There was only a slight improvement in the efficacy with deeper pathologies.
Later, we moved on to higher powered lasers and began to achieve better results. However, it was very time consuming to put the energy in slow enough not to burn the tissue and to cover all affected areas. Although results improved, they were still limited when treating deeper pathologies.
We began to experiment with multiple diode lasers at higher powers, now delivering two thousand milliwatts. of power. These high powered diode lasers gave us amazing results for the first few patients, but as the lasers heated up, they lost efficacy. The higher powered lasers delivered through a fiber optic system seemed to create excessive heat and were also not very useful for deep tissues or acute pathologies.
In fact, we achieved miraculous results with our multiple diode medium powered systems where each diode was only 500 milliwatts. However, after two or three treatments these laser heads became too hot and much less effective.
Knowing that there must be a reason for the cooler laser success and the hot high powered laser failure, Dr. Frederick took the only laser fundamentals course offered in the USA. It was through the American Surgical and Medical laser society that he gained the knowledge and understanding that lead to the development of the AHL laser protocols.
Additionally, Dr. Frederick gained invaluable insight from one of his patients who is a world famous plastic surgeon. This individual enlightened Dr. Frederick about a surgical cooling system that can cool the laser head and skin surface simultaneously. By regulating the surface temperature, Dr. Frederick is able to avoid damaging tissues while using higher powers.
Subsequently Dr. Frederick also discovered a laser in Italy that has a computer control system that takes into account thermal tissue relaxation times. The laser can be set up to increase cooling times and put the energy in at very high powers, hundreds of times greater than diode lasers. With peak powers of 3 million milliwatts of power and limited to no risk of tissue overheating, the deepest of pathologies can now be reached.
With the longest wavelength, highest power, and external cooling system, a new dimension exists that no other therapeutic laser device is capable of delivering. A photoacoustic wave can now be generated which creates enough pressure to reduce inflammation by forcing it into the lymphatic system. Furthermore the pressure wave can be used to actively release muscle spasms.
AHL’s external cooling coupled with high level laser application allows for acute photocoagulation to stop acute profusion of bleeding immediately thus greatly reducing the time of recovery from traumatic injuries such as those incurred in professional sports.
Dr. Frederick and AHL have flown across the country to help professional athletes and the athletes also fly across the country to be treated with the amazing AHL therapeutic laser system.
Currently, Dr. Frederick lectures on therapeutic laser treatments and protocols, and trains other medical professionals so they may offer the same amazing results for injuries and pain management. Once medical professionals complete the AHL Therapeutic Laser certification course, they are eligible to join the AHL certified professional program.
- Laser light waves can penetrate the skin with no heating effect, no damage to skin & no side effects
- Laser light directs biostimulative light energy to the body’s cells which convert into chemical energy to promote natural healing & pain relief
- LASER optimizes the immune responses of blood & has anti-inflammatory & immunosuppressive effects
- Laser light waves increase cellular regeneration
- This involves the physiology of cell metabolism, the mitochondria and the synthesis of ATP
- Laser light waves increase cellular communication
- This involves the nervous system, phospholipid cell membrane and the integrin system
- Important photon receptors on the phospholipid cell membrane called integrins link the cellular matrix with the extra-cellular matrix and all of the connective tissue. When the Laser light hits these receptors, it triggers a chain reaction of photon emissions to other cells which cascades through the body.
Physiological Effects
- Laser light directs biostimulative light energy to the body’s cells which convert into chemical energy to promote natural healing & pain relief
- Biostimulation: improved metabolism, increase of cell metabolism (increases speed, quality and tensile strength of tissue repair
- Improves blood circulation and vasodilation, increasing blood supply
- Increases ATP production (energy): ATP is used to drive cell metabolism (maintain membrane potentials; synthesize proteins; and power cell motility and replication)
- Optimizes the immune responses of blood & has anti-inflammatory & immunosuppressive effects.
- Increase cellular regeneration by involving the physiology of cell metabolism, the mitochondria and the synthesis of ATP
- Increases cellular communication, by involving the nervous system, phospholipid cell membrane and the integrin system
- Important photon receptors on the phospholipid cell membrane called integrins link the cellular matrix with the extra-cellular matrix and all of the connective tissue. When the Laser light hits these receptors, it triggers a chain reaction of photon emissions to other cells which cascades through the body.
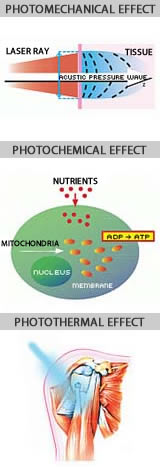
The exact mechanisms on how laser work on tissue is very well documented in hundreds of studies and we will try to give a simplified explanation. But make no mistake, laser energy is a very powerful tool and only those who have been properly trained should operate high powered lasers.
When tissues are hit with a laser, the light or photonic energy is either reflected, scattered, goes through without absorption or is absorbed. In general the tissue must absorb the light energy in order for it to be effected.
In traditional laser therapy we are most concerned about the photochemical effect. That is also the most researched effect.
The photochemical effect begins when a photoacceptor absorbs photonic energy. An example of a photoacceptor in plants is chlorophyll. In the human body we have non-specialized photoacceptors molecules, meaning the function is not dependent on light but is affected. Once a molecule has absorbed the light it can cause a wide variety of functions to be activated.
As a side, another use of lasers that is quickly developing is PDT (Photo Dynamic Therapy). In this case a photoacceptor is injected into tumor cells and a laser can then be used to target the tumor tissue only. We will not be talking about this in any detail. However, there is a possibility in the future that by adding a photoacceptor, in the future we may be able to specifically activate stem cells to produce new ligaments, muscles and tendons. This is not available at this time.
Irradiation of cells at certain wavelengths can also activate some of the native components. In this way specific biochemical reactions as well as cellular metabolism can be altered. This type of reaction is the basis of certainly low level laser and, in part, high intensity laser therapy. One should note that light therapy methods based on photochemical conversion of photo absorbing molecules are not necessarily laser specific. Meaning other sources of light could also lead to these reactions. It is the lasers ability to penetrate that makes it the most practical tool for delivery, especially when the tissue is deep.
Specific data on the effects of irradiated on various cells have been reviewed, including: cell cultures in vitro (13, 14) and human lymphocytes (17, 18). In addition clinical applications and research documentation included on the research tab are the sources of our information.
Again when I say photoacceptor here, I will be referring to non-specific molecular absorption. After absorbing the light, the molecule assumes an electronically excited state from which primary molecular processes can lead to a measured biological effect. To work as a photoacceptor taking part in photobioregulation, this molecule must be part of a key structure that can regulate a metabolic pathway. Redox chains are an example of this type of key structure which fits these requirements.
Several pieces of evidence show that the mitochondria are sensitive to irradiation with monochromatic visible and infrared light (IR). The illumination of isolated rat liver mitochondria increased adenosine triphosphate (ATP) synthesis and the consumption of oxygen. (23-25). Irradiation with light also increased the mitochondrial membrane potential and proton gradient, caused changes in the mitochondrial optical properties and modified some NADH-linked dehydrogenase reactions (NADH is a reduced form of nicotinamide adenine dinucleotide) and increased the rate of ADP/ATP exchange(28), as well as RNA and protein synthesis in the mitochondria.
These results were interpreted as definitely affecting mitochondria in an anabolic way. The question is which molecule in the mitochondria is responsible for the effects mentioned above. When considering the cellular effects, this question can be answered with the aid of action spectra. We know that within certain limits an action spectra follows the absorption spectrum of the photoacceptor molecule (28).
The results conclude that all bands in the action spectrum are related to the cytochrome C-Oxidase. The fact that the photoacceptors are components of the respiratory chain makes it easy to understand why ATP production is affected. Cytochrome c oxidase is a terminal enzyme of the respiratory chain, which mediates the transfer of electrons from cyt c to molecular oxygen. Ferrocytochrome c is oxidized, dioxygen is reduced, and protons are pumped vectorially from the mitochondrial matrix to the cytosol. Free energy resulting from this redox chemistry is converted into an electrochemical potential across the inner membrane of the mitochondrion, which ultimately drives the production of ATP. Accordingly, cytochrome c-oxidase plays a central role in the bioenergetics of the cell.

 Visit us on Facebook!
Visit us on Facebook!